Originally published in the 2019 winter issue of American Fitness Magazine
Humans seem to be prone to many different syndromes. One definition of the word syndrome on Merriam-Webster.com is “a group of signs and symptoms that occur together and characterize a particular abnormality or condition.”
Interestingly, the second definition listed is “a set of concurrent things . . . that usually form an identifiable pattern.” As corrective exercise professionals, we can identify a variety of “signs and symptoms” of physical syndromes by looking for an “identifiable pattern” in human movement.
The more common syndromes discussed in the realm of human movement include patellofemoral pain syndrome, subacromial impingement syndrome, myofascial pain syndrome, iliotibial band syndrome, and the well-known upper crossed and lower crossed syndromes. It’s important to highlight that these syndromes do not manifest overnight; they stem from patterns of movement impairments, called movement syndromes.
Movement syndromes were first described by Vladimir Janda, MD, DSc, a Czech medical doctor who dedicated his life to the study of pain syndromes and was known to many as the father of rehabilitation.
Over years of observing both his patients and the general public, Janda noticed that many people demonstrated similar patterns of impairment, which led him in 1979 to define three basic compensatory patterns: upper crossed syndrome, lower crossed syndrome and a combination of both (Page, Frank & Lardner 2010). It was not until later that pronation distortion syndrome emerged as a movement syndrome to look out for in assessments.
Today, unfortunately, PDS is still not discussed very frequently in the scientific literature, even though the topic is addressed in many blogs and newsletters. Despite the paucity of research, however, fitness professionals are likely to encounter PDS, so it is helpful to know what it looks like and what you can do about it if you spot the signs.
Because movement syndromes predictably lead to patterns of injury, fitness pros can help clients avoid pain and setbacks by learning more about identifying impaired movement patterns during assessments—and addressing those patterns appropriately in exercise programming.
Signs and Causes of PDS
PDS is characterized by excessive pronation of the foot along with simultaneous knee flexion and femoral internal rotation and adduction (see “A Pronation Primer,” below, for a quick review). In layperson speak, a person with PDS may be described as flat-footed and knock-kneed (Lucett 2013; NASM 2014). Foot dysfunction is often the initial cause of this posture, but it can also be attributable to hip dysfunction.
PDS AND FOOT DYSFUNCTION. In standing position, a flat foot causes the tibia to rotate internally, which in turn results in the femur rotating internally (since the femur rests on top of the tibia). This femoral internal rotation (also in standing position) causes simultaneous adduction. Such a response is referred to as obligatory joint motion and occurs in closed-chain movements (NASM 2014).
PDS AND HIP DYSFUNCTION. When there is hip dysfunction (e.g., weakness in the abductors, such as the gluteus medius), the femur may begin to rotate and adduct, eventually leading to foot pronation.
Both of these are cases of PDS, but each has a different origin of dysfunction. Fitness professionals must determine where a client’s dysfunction derives from in order to design the most appropriate program.
Negative Effects of PDS
While some pronation is normal and necessary in the foot and ankle complex (see “A Pronation Primer”), too much of it leads to injury and pain.
INJURIES TO THE FOOT AND ANKLE
PDS can cause pain local to the foot, ankle and lower leg. Potential types of pain include general foot and toe pain, plantar fasciitis, Achilles tendinopathy, posterior tibialis tendinitis, and anterior tibialis tendinitis (NASM 2014). Some research has found a strong association between PDS and lower-body overuse injuries like those just mentioned (Fong et al. 2008).
Overuse injuries generally develop when stress placed on the structures and tissues of the foot and ankle is compounded with each step. Over time, tissues may become irritated, inflamed or even weakened, which often leads to more serious problems, such as ruptured tendons or stress fractures.
INJURIES TO THE KNEE, HIP AND LOWER BACK
Individuals with PDS may also be subject to knee, hip and lower-back pain. A common knee condition is patellar tendinitis (jumper’s and runner’s knee). Like the foot, the knee can be abnormally stressed during too much femoral internal rotation and adduction. Further, the position of knee valgus is closely associated with knee injuries such as noncontact ACL rupture (NASM 2014). Noncontact injuries are frequently equated with overuse injuries in that the tissues are weakened over time (usually owing to too much repetitive stress with no time for full recovery between stressing events). Similarly, PDS often shifts the hip out of proper alignment, causing general hip and lower-back pain.
Negative Influence on Movement and Performance
PDS not only increases the chances of certain aches, pains and injuries; it also has negative effects on overall movement and performance. As already mentioned, excessive pronation will misalign the entire lower body, reducing the ability of powerful muscles like the quadriceps and glutes to maintain force production. Length–tension relationships establish that the resting length of a muscle determines whether it can generate optimal tension (NASM 2018).
A muscle that is shorter or longer than ideal length will have a less-than-ideal contraction. When a muscle cannot do its job fully, then surrounding “helper” muscles pick up the slack. This is known as synergistic dominance (NASM 2018). Although this process helps individuals move from point A to point B, it does not guarantee that the movement is occurring in the best possible manner, so it may result in injury or cause performance to decrease.
Decreased performance can occur for a variety of reasons. One possibility is that the prime mover is not driving the movement. A second reason is that the alteration of skeletal alignment is causing a series of energy “leaks.” To do repetitive high jumps, for example, an athlete must land with feet, ankles, knees, hips, pelvis and spine in a stacked position. The stacked position loads extensible structures correctly, helping to keep the joints safe.
However, if the feet excessively flatten and the femur excessively rotates and adducts (as in PDS), then the joints don’t stack, the tissues don’t load, and energy is lost. Sometimes this means an athlete can demonstrate one high jump, but with each landing and subsequent jump, the height decreases. In this case, the decline in performance is not due to fatigue but due to the inability to load properly with each jump.

PDS is characterized by excessive pronation of the foot along with simultaneous knee flexion and femoral internal rotation and adduction. In layperson speak, that translates to flat feet and knock-knees.
Corrective Rationale for PDS
Pronation isn’t something that necessarily needs to be corrected. However, clients who excessively pronate, thereby altering the position of the entire lower body, are candidates for a PDS corrective exercise program. The goal is to first determine what body part may be causing the dysfunction (e.g., foot, ankle or hips). The overhead squat assessment can help with this.
STEP 1: OVERHEAD SQUAT ASSESSMENT
Have the client perform the OHSA.
- If the feet are straight and parallel, not flattened or externally rotated, the client is not experiencing too much pronation and is therefore not a likely PDS candidate.If the lateral portion of the foot (i.e., the fifth toe and metatarsal) raises or rotates off the floor, or if the kneecap moves inside the first toe, the client is experiencing excess pronation and medial movement. In this case, performing a modified OHSA can help identify the likely source of the problem.

STEP 2: OHSA WITH HEELS ELEVATED
Next, modify the squat by elevating the heels onto a block or weight plates. Lifting the heels takes the calves out of the equation.
- If the client demonstrates a better squat in this position (i.e., the metatarsals stay on the floor and the knee does not move medial to the first toe), then it is reasonable to assume that the muscles crossing the ankle are playing a significant role in the dysfunction. (See Program 1, below for corrective exercise suggestions.)If elevating the heels does not change the knee position during the squat, then the problem likely derives from some dysfunction in the hip complex. (See Program 2, below for corrective exercise suggestions.)

Putting PDS Into Practice
In summary, PDS is a common movement pattern that often results in pain and injury to the foot, ankle, knee and hip. Using the correct assessment process and designing an appropriate program can improve movement patterns in most clients. This, in turn, can help prevent the negative effects of PDS from occurring in the first place.
A Pronation Primer
Pronation can occur at many different places in the body, but it is commonly discussed with regard to the feet or hands. Pronation is not a bad thing. The human foot is designed to pronate as a way of reducing impact forces during walking and running (Neumann 2010).
WHY (SOME) PRONATION IS NECESSARY
When the heel strikes the ground, the foot pronates, allowing the bones of the midfoot to “open up” so the foot becomes a soft landing surface. Further, the powerful glute muscles decelerate internal rotation of the tibia and femur to allow ground reaction forces to be transmitted through the body.
After the heel strike and moving through midstance, the opposite leg swings forward, and the pelvis twists the femur, rotating the leg and thus helping the foot to supinate. With supination, the foot starts to “wind up,” becoming a rigid, level surface for force propulsion. Thus, pronation and supination are mandatory for normal human movement.
WHEN PRONATION BECOMES A PROBLEM
The trouble begins when there is too much pronation, often referred to as overpronation, upon foot strike. While overpronation is less than ideal, so is not pronating.
PRONATION CONTROL IN FOOTWEAR
Pronation quality should always be considered when purchasing shoes, as many manufacturers seem to reinforce the medial portion of the shoe to reduce or block natural foot movement. Reinforcement or pronation control should only be introduced if needed, based on a gait assessment performed by a qualified professional.
Note: The NASM Corrective Exercise Specialization covers how to perform a detailed gait assessment using a treadmill (NASM 2014). To learn more, read about what a corrective exercise specialist does.
Two Corrective Programs for Addressing PDS
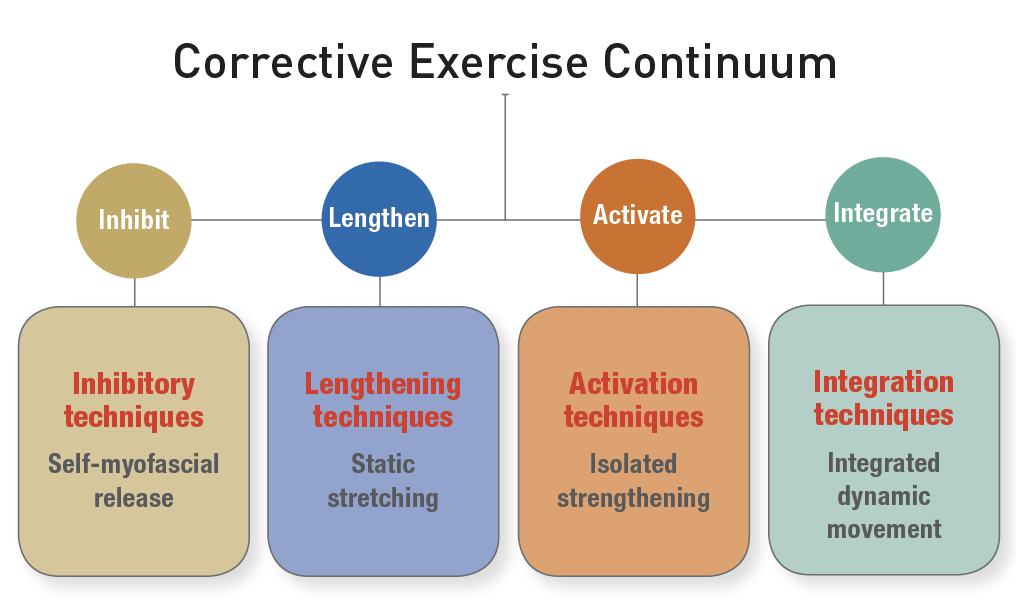
Once the primary cause of PDS has been identified, then a focused corrective exercise routine following the NASM Corrective Exercise Continuum can be implemented into the client’s general workout program.
PROGRAM 1: SAMPLE PDS ROUTINE FOR FOOT/ANKLE DYSFUNCTION
The goals of a foot/ankle corrective program are to be sure the ankle moves through an optimal range of motion and to improve the stability of the foot along with the alignment of the tibia. Try this program if elevating the heels improves the Overhead Squat Assessment results.
Inhibit / SMR
Perform 1 set each. Hold pressure on tender spots for 30–60 seconds.
>> plantar fascia
>> calves/gastrocnemius
>> peroneals

Lengthen / Static Stretching
Perform 2 sets, holding each for 30 seconds.
>> calves: static gastrocnemius stretch (standing wall stretch)
>> peroneals: standing stretch with abduction

Activate
Perform 1–2 sets of 12–20 reps with a slow tempo.
>> intrinsic foot: short foot/towel scrunches (When doing the towel scrunch, focus on activating the arch rather than just the toes.)
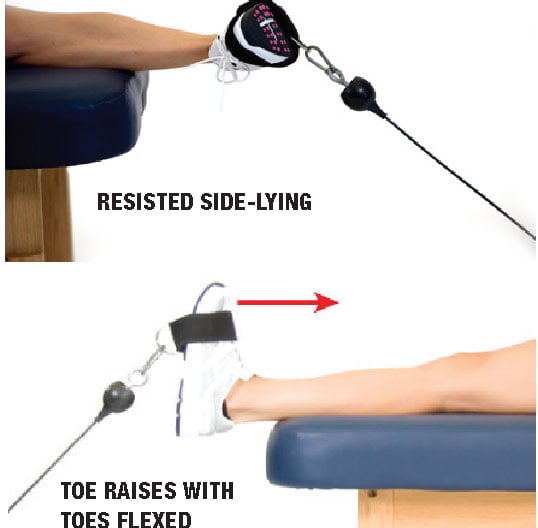
>> posterior tibialis: resisted side-lying
>> anterior tibialis: toe raises with toes flexed

Integrate
Perform up to 2 sets of 12–20 reps with a slow tempo.
>> single-leg balance with reach
>> reverse lunge with knee abduction

 PROGRAM 2: PDS PROGRAM FOR HIP COMPLEX DYSFUNCTION
PROGRAM 2: PDS PROGRAM FOR HIP COMPLEX DYSFUNCTION
The goals of the hip corrective program are to improve hip abduction, extension and external rotation and to increase stability and strength in the core and hip muscles. (Note: Try this program if elevating the heels does not improve the OHSA results.)
Inhibit / SMR
Perform 1 set on each part for 30–60 seconds. Hold pressure on tender spots.
>> adductors
>> tensor fasciae latae
>> quadriceps
Lengthen / Static Stretching
Perform 2 sets, holding each for 30 seconds.
>> adductors: standing static stretch with abduction
>> quads/hip flexors: static kneeling hip flexor stretch

Activate
Perform 1–2 sets of 12–20 reps with a slow tempo.
>> intrinsic core: plank (iso-abs)
>> hip external rotators: (press feet together) prone external rotation
>> gluteus medius: side-lying leg raise
>> gluteus maximus: ball bridge or floor bridge (with mini band)

Integrate
Perform up to 2 sets of 12–20 reps with a slow tempo.
>> single-leg balance with reach
>> lateral tube walking
>> reverse lunge with opposite reach


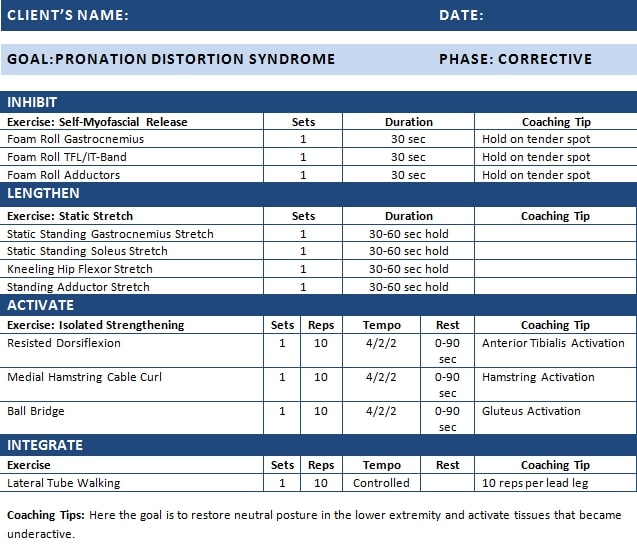
A sample workout for pronation distortion syndrome clients
Here is an additional reference to utilize for corrective exercise programming ideas for clients:
REFERENCES
Fong, D.T.P., et al. 2008. Effect of medial arch-heel support in inserts on reducing ankle eversion: A biomechanics study. Journal of Orthopaedic Surgery and Research, 3 (7).
Lucett, S. 2013. The effects of pronation distortion syndrome and solutions for injury prevention. Accessed Oct. 31, 2018: blog.nasm.org/fitness/the-effects-of-pronation-distortion-syndrome-and-solutions-for-injury-prevention/.
Merriam-Webster. 2018. Syndrome. Accessed Oct. 25, 2018: merriam-webster.com/dictionary/syndrome.
NASM (National Academy of Sports Medicine). 2014. NASM Essentials of Corrective Exercise Training (1st ed.). Burlington, MA: Jones & Bartlett Learning.
NASM. 2018. NASM Essentials of Personal Fitness Training (6th ed.). Burlington, MA: Jones & Bartlett Learning.
Neumann, D.A. 2010. Kinesiology of the Musculoskeletal System: Foundations for Rehabilitation (2nd ed.). St. Louis: Mosby Elsevier.
Page, P., Frank, C.C., & Lardner, R. 2010. Assessment and Treatment of Muscle Imbalance: The Janda Approach. Champaign, IL: Human Kinetics.

















